Harnessing the Heat: Nature’s Fiery Solution to Pain
Kaitlin Raskin
Illustrations by Mischa Landgarten & Iris Li
Millions of years of evolution have led chili pepper plants from Central and South America to possess a clever pain-inducing mechanism that deters pesky animals from eating them [1]. However, one species simply hasn’t gotten the hint: humans. They chewed on the fruit of the chili pepper plant and, despite feeling pain, they enjoyed it. Humans have since harnessed the plant’s active spicy ingredient, capsaicin, for culinary and medicinal purposes. Capsaicin naturally occurs in plants in the genus Capsicum, playing an important role in seed germination and protection from parasites since aversion to consuming capsaicin typically deters animals from eating Capsicum plants [1]. Besides its notable utility in the culinary world, capsaicin is also found in self-defense products such as pepper spray and has been traditionally used in medicine to relieve coughs and sore throats [2]. The interaction between capsaicin and the nervous system not only influences physiological responses to spicy food but also offers potential for pain relief [3, 4]. Hence, capsaicin is a promising alternative for treating chronic pain conditions, especially given the limited effectiveness and adverse side effects of many current pain medications [4, 5, 6].
Why is it spicy?
When we eat spicy food, capsaicin molecules bind to and activate cell receptors responsible for receiving and processing pain signals [7]. Specifically, capsaicin activates transient receptor potential vanilloid 1 (TRPV1) receptors, which are found in nociceptive, or pain-sensing, neurons located in areas like the mouth, tongue, and skin [7, 8]. TRPV1 receptors are also activated by hot foods and beverages, linking the experiences of eating hot and spicy food [7]. When capsaicin binds to TRPV1 receptors, the molecule causes nociceptive neurons to fire, triggering the release of substance P and other pain-related signaling molecules from sensory nerve endings [9]. The signaling molecules travel through the body, relaying the pain signal to other neurons and eventually reaching the brain [1].
Through the pain-signaling cascade, capsaicin stimulates the autonomic nervous system, which is constantly regulating essential bodily functions, such as heart rate and breathing [10, 11]. Capsaicin triggers the ‘fight or flight’ response from the sympathetic nervous system (SNS), a branch of the autonomic nervous system that helps the body respond to stressful stimuli [11]. When eating a seemingly harmless taco on Taco Tuesday, a jalapeño may activate your SNS, leading to increased heart rate, perspiration, and a burning pain sensation in your mouth [12]. Since capsaicin and hot food activate heat and pain-sensing TRPV1 receptors, both stimuli can trick the nervous system into thinking the body is overheating [13]. Like putting out a fire, the brain relays signals to the body to activate bodily cooling mechanisms [10, 14, 15]. Autonomic responses like increased sweating, salivation, and blood flow can occur as a result of the jalapeño [10, 14, 15]. Physiological responses to the pain-signaling cascade may consequently lead you to try to reduce the pain and alleviate these symptoms [10, 14]
Picture yourself eagerly preparing a fiery bowl of spicy Buldak Ramen for dinner. You take a bite and are immediately hit with a wave of pain as you begin to sweat, and your mouth waters ferociously — what do you do next? Your first instinct is to gulp down the glass of water next to you to alleviate the pain. Unfortunately, water doesn’t work because capsaicin is a hydrophobic substance, meaning it does not dissolve in water [16]. Pivoting to plan B, you frantically pour and drink a glass of milk, experiencing relief as the heat dissipates. Milk contains relatively hydrophobic casein molecules that surround and isolate the hydrophobic capsaicin molecules from the TRPV1 receptors [16, 17]. Similar to how soap washes away grease, the casein molecules effectively wash away the capsaicin, alleviating the capsaicin-induced burning sensation [16, 18].
The Capsaicin Pleasure-Pain Paradox
If spicy food causes pain, why would someone ever choose to eat Flamin’ Hot Cheetos instead of regular Cheetos? After spicy food activates nociceptive neurons and causes a pain response, the body tries to counteract the pain signals by releasing pain-relieving molecules called endorphins [19]. Endorphins are hormones that are secreted by the pituitary gland, an area of the brain responsible for producing hormones that indirectly regulate many bodily functions such as growth and metabolism [20, 21]. Endorphins bind to opioid receptors, which are also the targets for pain-relieving opioid drugs like morphine [20]. When endorphins bind to opioid receptors, they prevent the release of pain-signaling molecules like substance P, reducing the sensation of pain [19, 22, 23]. In the brain and spinal cord, endorphins also stimulate an increase in dopamine, a chemical messenger transmitted between cells in the brain’s reward system [19]. The feeling of reward associated with dopamine release is a central motivating factor in our consumption of spicy food [19, 24]. Through the release of endorphins and dopamine, spicy food contributes to feelings of euphoria and leaves us wanting more, which may explain why some people choose to eat Flamin’ Hot Cheetos despite the subsequent pain responses [24].
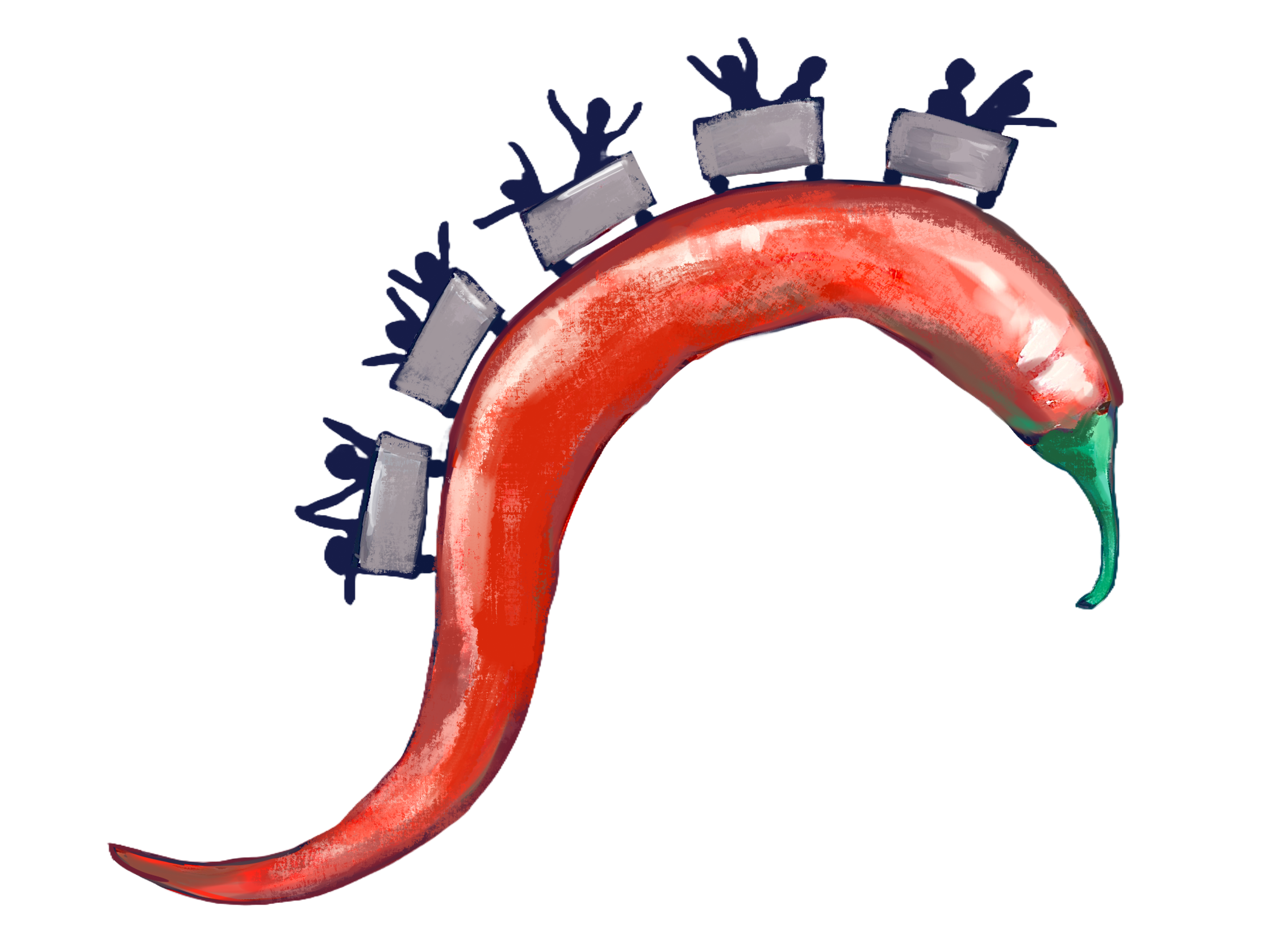
On an individual level, personality traits also influence whether or not someone enjoys eating spicy food [25, 26]. Imagine you are at an amusement park, deciding between riding the roller coaster or the carousel. You choose the carousel, preferring a familiar and gentle experience over the excitement and unpredictability of the roller coaster. Consistently choosing the carousel over the rollercoaster can reflect a dislike of unfamiliar experiences. Similarly, individuals who don’t like spicy food are often more reluctant to try unfamiliar dishes [27]. People who don’t like spicy food are also more likely to experience disgust, responding more negatively to offensive stimuli such as rotten food and bodily fluids [27]. Those who dislike spicy food also tend to exhibit heightened reactions to negative consequences and are less motivated to seek out novel and complex experiences that produce feelings of reward [27, 28]. Now, imagine you had instead chosen to ride the roller coaster, finding thrill in unexpected acceleration changes and gravity-defying plunges. Individuals with greater sensitivity to feelings of reward are also generally more likely to enjoy eating spicy food [25, 26, 29]. Just as personality influences our choice of amusement park rides, it also plays a significant role in our food preferences, with risk-taking and sensitivity to reward often driving the enjoyment of spicy foods [26, 29]. But even if you tend to prefer the carousel and avoid taking risks, there is still hope for developing a tolerance and finding enjoyment in spicy food [30].
Burning Away the Pain
Repeated consumption of spicy foods can lead to desensitization, a process in which the painful sensations triggered by capsaicin diminish [30]. Suppose you decide to challenge yourself by ordering Buffalo Wild Wings with Mango Habanero sauce every day for two weeks. For the first few days of the challenge, the heat from the sauce is unbearable, and your mouth is on fire. However, the spice level begins to feel tolerable over the course of the two-week period, and you start to fully appreciate the sweetness and complex flavors of the spicy sauce [1, 2, 30]. You experience a reduced pain response because consuming capsaicin at high doses or with prolonged exposure can lead to desensitization of the TRPV1 receptor pathway [1, 2, 30]. Constant activation of TRPV1 receptors by capsaicin or painful heat desensitizes the receptors for extended periods of time, preventing nociceptive neurons from firing [2]. As a result, there is a decrease in responses like sweating and salivation to a variety of TRPV1-related pain stimuli [1, 2, 30]. Additionally, when capsaicin repeatedly binds to TRPV1 receptors, an abundance of substance P pain-signaling molecules are released from nociceptive neurons [1, 2]. Once the supply of substance P becomes exhausted, the nociceptive neurons become functionally silent as they can no longer communicate pain signals to the brain [1, 2]. Preventing the spread of the pain-signaling cascade contributes to TRPV1 desensitization [1, 2]. After being successfully desensitized to the spiciness of Mango Habanero sauce, you then take a year-long hiatus from eating spicy wings before ordering some more. You’re certain that you will be able to handle the spice as you did before. However, upon consumption, you are shocked to find that, yet again, your mouth is burning, and your eyes are watering. Unfortunately, at low doses of capsaicin, desensitization must be maintained by eating spicy food on a somewhat regular basis [30]. Although capsaicin works to silence nociceptive neurons, explaining the initial desensitization, the molecule simultaneously triggers the growth and regeneration of these neurons through a different signaling pathway [30, 31, 32]. Capsaicin binds to TRPV1 receptors, causing calcium ions to rush into the neurons and initiate a signaling cascade that activates a protein involved in growth and repair [32]. Once the neurons are repaired after several weeks or months, they may return to transmitting pain signals through the spinal cord and to the brain, causing a return of sensitivity to the Mango Habanero sauce [31, 32].
Capsaicin’s ability to induce desensitization by impairing TRPV1 receptors and silencing nociceptive neurons allows the molecule to be used pharmacologically to treat various pain conditions [1, 2]. TRPV1 receptors are not only located in areas that come into contact with food, such as the mouth, but also throughout the body as part of the peripheral nervous system, which allows neural signals to be sent between the rest of the body and the brain and spinal cord [33]. Thus, the pain-relieving properties of capsaicin can extend beyond the realm of culinary experiences and can be effectively utilized in clinical settings [32]. Capsaicin treatment can be used to facilitate pain relief for those suffering from neuropathic pain [2]. Neuropathic pain refers to pain stemming from nerve damage, which arises from disorders affecting sensory nerves [32, 34]. Affecting roughly 7-10% of the global population, neuropathic pain disorders include diabetic neuropathy as well as chronic pain and phantom limb pain (PLP) [2, 32]. Neuropathic pain for people with diabetic neuropathy, in which elevated blood sugar levels lead to nerve damage, often takes the form of a persistent pinching feeling in their legs and feet [35]. Moreover, individuals with amputated limbs often report experiencing PLP, which refers to an unexplainable stabbing or tingling sensation that seems to originate from the missing limb [36, 37, 38]. Neuropathic pain disorders are often difficult to treat due to the variability underlying nerve damage and dysfunction [39]. However, capsaicin provides a unique approach to complex diagnoses by inducing pain desensitization [3, 4].
Unlike pre-existing treatments for neuropathic pain disorders, capsaicin offers an alternative avenue for pain management through the skin [2, 32]. Capsaicin is commonly used as an ingredient in topical formulations, meaning it is applied directly to the skin with a patch or as a cream [2, 32]. Though capsaicin application to the skin initially increases pain sensitivity through TRPV1 receptor activation, high concentrations or repeated applications of topical capsaicin can lead to persistent pain desensitization [33]. As a result, pain signals are prevented from reaching the brain, alleviating pain over time [2, 3, 34]. Medications utilizing capsaicin are unique in that they work through the peripheral nervous system, more directly targeting nerves in an affected area [40, 41]. In contrast, many long-standing medications for disorders like diabetic neuropathy, such as antidepressants and anticonvulsants, act through the central nervous system to interfere with pain processing in the brain and spinal cord [40, 41, 42, 43].
Since antidepressants and anticonvulsants don’t treat one specific area of pain, multiple neurotransmitter systems are affected, which can contribute to side effects [44]. While antidepressants and anticonvulsants have been traditionally used to treat depression and seizures, they’ve also been established as effective first-line treatments for diabetic neuropathy [44, 45]. However, these medications are associated with a myriad of adverse side effects, including dry mouth, constipation, dizziness, and headaches [44, 45]. Opioids, which may be administered when first-line treatments are ineffective in reducing pain, are also risky, potentially leading to addiction and abuse [32]. In comparison, topical capsaicin therapies provide an alternative form of treatment that circumvents many potential risks and side effects [45]. When a high concentration of topical capsaicin formula was applied to the feet of people with diabetic neuropathy, the pain was significantly reduced over two months [45, 46]. However, capsaicin administration was still associated with a burning sensation and pain at the application site despite the application of a local anesthetic before treatment [34, 44, 45, 46]. Fortunately, this pain dissipates over time following the initial administration. The pain relief from a high concentration of topical capsaicin is long-lasting, persisting up to three months after one application [44, 47]. Relative to an anticonvulsant, topical capsaicin treatments provide pain relief with a faster onset of action, greater patient satisfaction, and fewer side effects [46]. As a result, in 2020, the Food and Drug Administration approved topical capsaicin as a treatment for diabetic neuropathy [45]. Like diabetic neuropathy treatments, antidepressant and anticonvulsant treatments for chronic PLP in people with amputations have been criticized for their associations with similar side effects [38, 48]. In contrast, a highly concentrated topical capsaicin patch applied to the amputation stump was found not only to reduce the intensity of both chronic pain at the site of the stump and PLP from the missing limb, but also to help a patient’s brain recognize that the limb where they once felt pain is gone [38, 48]. For people who have had leg amputations, attempting to use prostheses can lead to more stump pain when walking [38, 48]. Capsaicin is therefore beneficial for reducing pain while also enabling amputees to use prosthetics during the rehabilitation process [38, 48]. Ultimately, topical capsaicin offers a novel alternative with no significant adverse effects relative to traditional pharmacological treatments for pain management in people with amputations [38].
Flamin’ Hot Healin’
In a single bite of a spicy meal, the blazing heat from capsaicin molecules can not only ignite the sensation of fiery pain but also spark our understanding of unique pain treatments. By activating TRPV1 receptors, capsaicin triggers a cascade of pain signals that engage the body’s autonomic nervous system, producing responses like sweating and increased heart rate [11]. Yet, paradoxically, the initial pain is often met with pleasure due to the release of endorphins and dopamine, explaining why many enjoy consuming spicy food [24]. Along with helping to build tolerance to spicy food, capsaicin’s ability to induce desensitization through pain pathway interference underscores its therapeutic potential for neuropathic pain conditions such as diabetic neuropathy and phantom limb pain [3, 4]. By targeting pain directly in the affected areas, capsaicin-based therapies provide a novel alternative to conventional medications with fewer side effects and greater patient satisfaction [46]. So the next time you decide to turn up the heat with a fiery curry or hot salsa, embrace the burn while savoring the science behind it!
References
Fattori, V., Hohmann, M. S. N., Rossaneis, A. C., Pinho-Ribeiro, F. A., & Verri, W. A. (2016). Capsaicin: Current understanding of its mechanisms and therapy of pain and other pre-clinical and clinical uses. Molecules, 21(7), 844. doi:10.3390/molecules21070844
Basith, S., Cui, M., Hong, S., & Choi, S. (2016). Harnessing the therapeutic potential of capsaicin and its analogues in pain and other diseases. Molecules, 21(8), 966. doi:10.3390/molecules21080966
Thomas SE, Laycock H. (2020). The use of high dose topical capsaicin in the management of peripheral neuropathy: narrative review and local experience. Br J Pain, 14(2), 133-140. doi: 10.1177/2049463720914332
Finnerup, N. B., Attal, N., Haroutounian, S., McNicol, E., Baron, R., Dworkin, R. H., Gilron, I., Haanpää, M., Hansson, P., Jensen, T. S., Kamerman, P. R., Lund, K., Moore, A., Raja, S. N., Rice, A. S. C., Rowbotham, M., Sena, E., Siddall, P., Smith, B. H., & Wallace, M. (2015). Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. The Lancet Neurology, 14(2), 162–173. doi:10.1016/s1474-4422(14)70251-0
Staelin R., Koneru, S. N., & Rawe, I. M. (2017) An over-the-counter central sensitization therapy: A chronic back pain registry study of pain relief, medication use and their adverse effects, Pain Management, 7:2, 99-111. doi:10.2217/pmt-2016-0046
Scott, N.L. & Miner, J.R. (2016) The safe and rational use of analgesics: Non-opioid analgesics. Curr Emerg Hosp Med Rep 4, 66–70 (2016). doi: 10.1007/s40138-016-0102-5
Mickle, A. D., Shepherd, A. J., & Mohapatra, D. P. (2016). Nociceptive TRP Channels: Sensory detectors and transducers in multiple pain pathologies. Pharmaceuticals, 9(4), 72. doi:10.3390/ph9040072
Fischer MJM, Ciotu CI and Szallasi A (2020) The mysteries of capsaicin-sensitive afferents. Front. Physiol. 11, 554195. doi:10.3389/fphys.2020.554195
Frias, B., & Merighi, A. (2016). Capsaicin, nociception and pain. Molecules, 21(6), 797. doi:10.3390/molecules21060797
Kawakami, S., Sato, H., Sasaki, A. T., Tanabe, H. C., Yoshida, Y., Saito, M., Toyoda, H., Sadato, N., & Kang, Y. (2016). The brain mechanisms underlying the perception of pungent taste of capsaicin and the subsequent autonomic responses. Frontiers in Human Neuroscience, 9, 720. doi:10.3389/fnhum.2015.00720
Mulkey, S.B. & du Plessis, A.J. (2019) Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatr Res 85, 120–126. doi:10.1038/s41390-018-0155-0
Scott-Solomon, E., Boehm, E. & Kuruvilla, R. (2021) The sympathetic nervous system in development and disease. Nat Rev Neurosci 22, 685–702. doi:10.1038/s41583-021-00523-y
Szolcsányi, J. (2015). Effect of capsaicin on thermoregulation: an update with new aspects. Temperature, 2(2), 277–296. doi:10.1080/23328940.2015.1048928
Kono, Y., Kubota, A., Taira, M., Katsuyama, N. & Sugimoto, K. (2018). Effects of oral stimulation with capsaicin on salivary secretion and neural activities in the autonomic system and the brain. Journal of Dental Sciences, 13(2), 116-123. doi:10.1016/j.jds.2017.08.007
Michlig, S., Merlini, J., Beaumont, M. et al. Effects of TRP channel agonist ingestion on metabolism and autonomic nervous system in a randomized clinical trial of healthy subjects. Sci Rep 6, 20795 (2016). doi:10.1038/srep20795
Gaiser, J., & Hayes, J. E. (2023). More than fat – Proteins in dairy and plant milks contribute to the reduction of oral burn from capsaicin. Food Quality and Preference, 112, 105041. doi:10.1016/j.foodqual.2023.105041
Nolden, A. A., Lenart, G., & Hayes, J. E. (2019). Putting out the fire - Efficacy of common beverages in reducing oral burn from capsaicin. Physiology & behavior, 208, 112557. doi:10.1016/j.physbeh.2019.05.018
Farah, B. A., Hayes, J. E., & Coupland, J. N. (2022). The effect of dairy proteins on the oral burn of capsaicin. Journal of Food Science. doi:10.1111/1750-3841.16400
Choy, M., El Fassi, S., & Treur, J. (2021). An adaptive network model for pain and pleasure through spicy food and its desensitization. Cognitive Systems Research, 66, 211–220. doi:10.1016/j.cogsys.2020.10.006
Pilozzi, A., Carro, C., & Huang, X. (2021). Roles of β-endorphin in stress, behavior, neuroinflammation, and brain energy metabolism. International Journal of Molecular Sciences, 22(1), 338. doi:10.3390/ijms22010338
Ammar Abdulhasan Aldhalemi, & Lahhob, Q. R. (2024). The study of chemical reactions in the human body through the use of hormones. International Journal of Advanced Biochemistry Research, 8(5), 01–09. doi:10.33545/26174693.2024.v8.i5a.1048
Fairbanks, C. A. & Peterson, C. D. (2023). The opioid receptor: emergence through millennia of pharmaceutical sciences. Front. Pain Res. 4:960389. doi: 10.3389/fpain.2023.960389
Smutzer, G. & Devassy, R. K. (2016). Integrating TRPV1 receptor function with capsaicin psychophysics. Advances in Pharmacological Sciences, 1-16. doi:10.1155/2016/1512457
Berridge, K. C., & Robinson, T. E. (2016). Liking, wanting, and the incentive-sensitization theory of addiction. American Psychologist, 71(8), 670–679. doi:10.1037/amp0000059
Byrnes, N. K., & Hayes, J. E. (2015). Gender differences in the influence of personality traits on spicy food liking and intake. Food Quality and Preference, 42, 12–19. doi:10.1016/j.foodqual.2015.01.002
Byrnes, N. K., & Hayes, J. E. (2016). Behavioral measures of risk tasking, sensation seeking and sensitivity to reward may reflect different motivations for spicy food liking and consumption. Appetite, 103, 411–422. doi:10.1016/j.appet.2016.04.037
Spinelli, S., De Toffoli, A., Dinnella, C., Laureati, M., Pagliarini, E., Bendini, A., Braghieri, A., Gallina Toschi, T., Sinesio, F., Torri, L., Gasperi, F., Endrizzi, I., Magli, M., Borgogno, M., di Salvo, R., Favotto, S., Prescott, J., & Monteleone, E. (2018). Personality traits and gender influence liking and choice of food pungency. Food Quality and Preference, 66, 113–126. doi: 10.1016/j.foodqual.2018.01.014
Siebert, E., Lee, S.-Y., & Prescott, M. P. (2022). Chili pepper preference development and its impact on dietary intake: A narrative review. Frontiers in Nutrition, 9. doi:10.3389/fnut.2022.1039207
Wang, X., Geng, L., Qin, J., & Yao, S. (2023). The potential relationship between spicy taste and risk seeking. Judgment and Decision Making, 11(6), 547–553. doi:10.1017/s1930297500004769
Nolden, A. A., Lenart, G., Spielman, A. I., & Hayes, J. E. (2024). Inducible desensitization to capsaicin with repeated low-dose exposure in human volunteers. Physiology & Behavior, 275, 114447. doi:10.1016/j.physbeh.2023.114447
Wang, S., Bian, C., Yang, J., Arora, V., Gao, Y., Wei, F., & Chung, M.-K. (2020). Ablation of TRPV1+ Afferent Terminals by Capsaicin Mediates Long-Lasting Analgesia for Trigeminal Neuropathic Pain. Eneuro, 7(3), ENEURO.0118-20.2020. doi:10.1523/eneuro.0118-20.2020
Arora, V., Campbell, J. N., & Chung, M.-K. (2020). Fight fire with fire: Neurobiology of capsaicin-induced analgesia for chronic pain. Pharmacology & Therapeutics, 220, 107743. doi:10.1016/j.pharmthera.2020.107743
Xiao, T., Sun, M., Zhao, C., & Kang, J. (2023). TRPV1: A promising therapeutic target for skin aging and inflammatory skin diseases. Frontiers in Pharmacology, 14. doi:10.3389/fphar.2023.1037925
Derry, S., Rice, A. S., Cole, P., Tan, T., & Moore, R. A. (2017). Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database of Systematic Reviews, 1(1). doi:10.1002/14651858.cd007393.pub4
Pathak, R., Sachan, N., & Chandra, P. (2022). Mechanistic approach towards diabetic neuropathy screening techniques and future challenges: A Review. Biomedicine & Pharmacotherapy, 150, 113025. doi: 10.1016/j.biopha.2022.113025
Weiss T, Koehler H, Croy I. (2022) Pain and reorganization after amputation: Is interoceptive prediction a key? The Neuroscientist. 29(6), 665-675. doi:10.1177/10738584221112591
Kaur, A., & Guan, Y. (2018). Phantom limb pain: A literature review. Chinese Journal of Traumatology, 21(6), 366–368. doi:10.1016/j.cjtee.2018.04.006
Privitera, R., Birch, R., Sinisi, M., Mihaylov, I. R., Leech, R., & Anand, P. (2017). Capsaicin 8% patch treatment for amputation stump and Phantom Limb Pain: A clinical and functional MRI study. Journal of Pain Research, 10, 1623–1634. doi:10.2147/jpr.s140925
van Velzen, M., Dahan, A., & Niesters, M. (2020). Neuropathic pain: Challenges and opportunities. Frontiers in Pain Research, 1. doi:10.3389/fpain.2020.00001
Goodwin, B., Maanas Chiplunkar, Salerno, R., Coombs, K., Umar Sannoh, Shah, V., Averell, N., Usmaan Al-Shebab, & Janora, D. M. (2023). Topical capsaicin for the management of painful diabetic neuropathy: a narrative systematic review. Pain Management, 13(5), 309–316. doi:10.2217/pmt-2023-0006
Meacham K, Shepherd A, Mohapatra DP, Haroutounian S. (2017) Neuropathic pain: Central vs. peripheral mechanisms. Curr Pain Headache Rep., (6), 28. doi: 10.1007/s11916-017-0629-5
Cohen, K., Nataliya Shinkazh, Frank, J., Israel, I., & Fellner, C. (2015). Pharmacological Treatment Of Diabetic Peripheral Neuropathy. Pharmacy and Therapeutics, 40(6), 372. PMID:26045647
Obata H. (2017) Analgesic mechanisms of antidepressants for neuropathic pain. Int J Mol Sci, 18(11), 2483. doi:10.3390/ijms18112483
Thouaye, M., & Yalcin, I. (2023). Neuropathic pain: From actual pharmacological treatments to new therapeutic horizons. Pharmacology & Therapeutics, 251, 108546. doi:10.1016/j.pharmthera.2023.108546
Jang, H. N., & Oh, T. J. (2023). Pharmacological and nonpharmacological treatments for painful diabetic peripheral neuropathy. Diabetes & Metabolism Journal, 47(6). doi:10.4093/dmj.2023.0018
Simpson DM, Robinson-Papp J, Van J, Stoker M, Jacobs H, Snijder RJ, Schregardus DS, Long SK, Lambourg B, Katz N. (2017). Capsaicin 8% patch in painful diabetic peripheral neuropathy: A randomized, double-blind, placebo-controlled study. J Pain, 18(1). 42-53. doi:10.1016/j.jpain.2016.09.008
Landrum, O., Marcondes, L., Egharevba, T., & Gritsenko, K. (2023). Painful diabetic peripheral neuropathy of the feet: Integrating prescription-strength capsaicin into office procedures. Pain Management, 13(10), 613–626. doi:10.2217/pmt-2023-0028
Alalami, K., Goff, J., Grimson, H., Martin, O., McDonald, E., Mirza, T., Mistry, D., Ofodile, A., Raja, S., Shaker, T., Sleibi, D., & Forget, P. (2024). Does topical capsaicin affect the central nervous system in neuropathic pain? A narrative review. Pharmaceuticals, 17(7), 842. doi:10.3390/ph17070842